Treatment of astrocytoma will involve a neurosurgeon to remove the tumor, a neuropathologist to examine the tumor sample, and an oncologist to monitor the patient’s health and coordinate radiation therapy and chemotherapy if necessary. Nurses and radiation therapists will also play a role. After treatment, the patient may be followed up by a neurologist
The World Health Organization (WHO) system is the most common; it has four grades of increasing severity based on the appearance of the astrocytoma cells. Other methods of staging correspond fairly closely to the WHO system. Grades I and II are sometimes grouped together and referred to as low-grade astrocytomas. Over time, tumors may progress from a low-grade form with a relatively good prognosis to a higher grade form and poorer prognosis. Additionally, tumors may recur at a higher grade.
There are several different systems for staging astrocytomas.
Grade I Pilocytic Astrocytoma
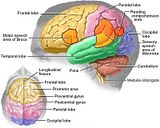
This is also sometimes referred to as juvenile astrocytoma because it occurs more frequently in children than adults. Under a microscope, the astrocytes are thin and elongated, and known as pilocytes. They are accompanied by Rosenthal fibers. The tumor mass does not invade surrounding tissues and is sometimes enclosed in a cyst. In children, pilocytic astrocytoma often occurs in the cerebellum, but may also occur in the cerebrum.
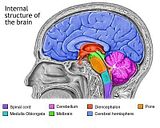
Treatment of this grade depends on the patient’s age and the location of the tumor. Surgery is the preferred treatment for this type of astrocytoma; it is performed by a procedure known as a craniotomy. An incision is made in the skin and an opening is made in the skull. After the tumor is removed, the bone is normally replaced and the incision closed. The neurosurgeon may also insert a shunt (drainage system) to relieve intracranial pressure; this involves inserting a catheter into a cavity inside the brain called a ventricle, then threading the other end under the skin to a drainage area where the fluid is absorbed. If the tumor can be completely surgically removed, the patient may not need further therapy and may be monitored only for recurrence.
If the tumor cannot be completely removed, patients may be given chemotherapy as well. If the tumor is not completely resected or if it continues to grow after chemotherapy, radiation therapy may be necessary. Radiation therapy is not normally given to children under the age of three in order to prevent permanent damage to the child’s healthy brain tissue. Radiation treatment may cause swelling in the brain; steroids may be prescribed to reduce the swelling. The best indicator for prognosis is complete removal of the tumor. With complete tumor removal, 80% of patients are alive ten years later. Location of the tumor in the cerebellum also suggests a better prognosis than other locations.
Grade II Low-Grade Diffuse Astrocytoma
These astrocytomas spread out and invade surrounding brain tissues but grow very slowly. Under the microscope, Grade II astrocytomas may occur anywhere in the brain, in the cerebellum and brain stem, or in the cerebrum, including the optic pathways. Genetic studies indicate that mutations of the tumor suppressor gene p53 occur frequently in these tumors. Surgical removal of the tumor is the first choice for treatment, but it may not be possible due the tumor’s location. Surgery is usually followed by radiation.
Patients under 35 years of age have a better prognosis than older patients; in older patients, low-grade tumors progress to higher grades more rapidly. Overall median survival is four to five years. Pleimorphic xanthoastrocytoma, a tumor originating in cells of a mixture of glial and neuronal origin, is often considered a grade II astrocytoma. It is relatively benign and treated only with surgery.
Grade III Anaplastic Astrocytoma
Anaplastic astrocytoma occurs most frequently in people aged 50 to 60. The term anaplastic means that the cells are not differentiated; they have the appearance of immature cells and cannot perform their proper functions. Researchers believe this is due to a gradual accumulation of genetic alterations in these cells. These tumor cells invade surrounding healthy brain tissue. Anaplastic astrocytomas may be inoperable because of their location and their infiltration into normal tissue; in this case radiation therapy is recommended. Chemotherapy may include various combinations of alkylating agents and other drugs, including carmustine, cisplatin, lomustine, procarbazine and vincristine.
These tumors tend to recur more frequently than grade I and II tumors. Following treatment, median survival is 12 to 18 months. The five-year survival rate for these patients is approximately 10% to 35%.
Grade IV Glioblastoma Multiforme
Glioblastoma Multiforme (GBM) is the most common primary brain tumor in adults. These tumors aggressively invade adjacent tissue and may even spread throughout the central nervous system. They frequently occur in the frontal lobes of the cerebrum.
KEY TERMS
Anaplastic—Undifferentiated, appearing to have an immature cell type.
Biopsy—A sample of tissue taken from the tumor.
Glioma—A tumor of the brain’s glial cells.
Primary tumor—An original tumor, not a metastatic tumor resulting from cancer’s spread. fibrous structures are present.
There are several different systems for staging astrocytomas.
Grade I Pilocytic Astrocytoma
This is also sometimes referred to as juvenile astrocytoma because it occurs more frequently in children than adults. Under a microscope, the astrocytes are thin and elongated, and known as pilocytes. They are accompanied by Rosenthal fibers. The tumor mass does not invade surrounding tissues and is sometimes enclosed in a cyst. In children, pilocytic astrocytoma often occurs in the cerebellum, but may also occur in the cerebrum.
Treatment of this grade depends on the patient’s age and the location of the tumor. Surgery is the preferred treatment for this type of astrocytoma; it is performed by a procedure known as a craniotomy. An incision is made in the skin and an opening is made in the skull. After the tumor is removed, the bone is normally replaced and the incision closed. The neurosurgeon may also insert a shunt (drainage system) to relieve intracranial pressure; this involves inserting a catheter into a cavity inside the brain called a ventricle, then threading the other end under the skin to a drainage area where the fluid is absorbed. If the tumor can be completely surgically removed, the patient may not need further therapy and may be monitored only for recurrence.
If the tumor cannot be completely removed, patients may be given chemotherapy as well. If the tumor is not completely resected or if it continues to grow after chemotherapy, radiation therapy may be necessary. Radiation therapy is not normally given to children under the age of three in order to prevent permanent damage to the child’s healthy brain tissue. Radiation treatment may cause swelling in the brain; steroids may be prescribed to reduce the swelling. The best indicator for prognosis is complete removal of the tumor. With complete tumor removal, 80% of patients are alive ten years later. Location of the tumor in the cerebellum also suggests a better prognosis than other locations.
Grade II Low-Grade Diffuse Astrocytoma
These astrocytomas spread out and invade surrounding brain tissues but grow very slowly. Under the microscope, Grade II astrocytomas may occur anywhere in the brain, in the cerebellum and brain stem, or in the cerebrum, including the optic pathways. Genetic studies indicate that mutations of the tumor suppressor gene p53 occur frequently in these tumors. Surgical removal of the tumor is the first choice for treatment, but it may not be possible due the tumor’s location. Surgery is usually followed by radiation.
Patients under 35 years of age have a better prognosis than older patients; in older patients, low-grade tumors progress to higher grades more rapidly. Overall median survival is four to five years. Pleimorphic xanthoastrocytoma, a tumor originating in cells of a mixture of glial and neuronal origin, is often considered a grade II astrocytoma. It is relatively benign and treated only with surgery.
Grade III Anaplastic Astrocytoma
Anaplastic astrocytoma occurs most frequently in people aged 50 to 60. The term anaplastic means that the cells are not differentiated; they have the appearance of immature cells and cannot perform their proper functions. Researchers believe this is due to a gradual accumulation of genetic alterations in these cells. These tumor cells invade surrounding healthy brain tissue. Anaplastic astrocytomas may be inoperable because of their location and their infiltration into normal tissue; in this case radiation therapy is recommended. Chemotherapy may include various combinations of alkylating agents and other drugs, including carmustine, cisplatin, lomustine, procarbazine and vincristine.
These tumors tend to recur more frequently than grade I and II tumors. Following treatment, median survival is 12 to 18 months. The five-year survival rate for these patients is approximately 10% to 35%.
Grade IV Glioblastoma Multiforme
Glioblastoma Multiforme (GBM) is the most common primary brain tumor in adults. These tumors aggressively invade adjacent tissue and may even spread throughout the central nervous system. They frequently occur in the frontal lobes of the cerebrum.
KEY TERMS
Anaplastic—Undifferentiated, appearing to have an immature cell type.
Biopsy—A sample of tissue taken from the tumor.
Glioma—A tumor of the brain’s glial cells.
Primary tumor—An original tumor, not a metastatic tumor resulting from cancer’s spread. fibrous structures are present.






0 comments:
Post a Comment